
Hello, I am Dr. Ayisha Livingstone, MD, a Fellowship trained and Board-Certified Orthopedic Hand Surgeon. I reside and practice in Fort Lauderdale, FL with the South Florida Orthopedic Group. I completed my Orthopedic Residency at the University of Miami, and my Fellowship at the University of Pittsburgh. I truly love my community here in South Florida and decided to help bring some awareness on some common hand and wrist ailments that present to my practice.
Trigger Finger/Thumb
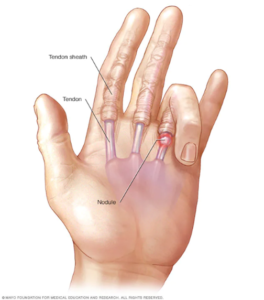
What is it…Trigger finger is also known as stenosing tenosynovitis (stuh-NO-sing ten-o-sin-o-VIE-tis). It occurs when inflammation narrows the space within the sheath that surrounds the tendon in the affected finger. If trigger finger is severe, your finger may become locked in a bent position. Trigger finger can affect any finger, including the thumb. More than one finger may be affected at a time, and both hands might be involved. Triggering is usually more pronounced in the morning, while firmly grasping an object or when straightening your finger.
Symptoms may include:
- A tender lump at the base of the finger on the palm side of the hand
- A catching, popping, or locking sensation with finger movement
- Pain when you bend or straighten the finger
- Difficulty fully flexing/bending your finger
Tendons are fibrous cords that attach muscle to bone. Each tendon is surrounded by a protective sheath. Trigger finger occurs when the affected finger’s tendon sheath becomes irritated and inflamed. This interferes with the normal gliding motion of the tendon through the sheath.
Prolonged irritation of the tendon sheath can produce scarring, thickening and the formation of bumps (nodules) in the tendon that impede the tendon’s motion even more.
Who can get it…People whose work or hobbies require repetitive gripping actions are at higher risk of developing trigger finger. The condition is also more common in women and in anyone with diabetes. Treatment of trigger finger varies depending on the severity.
Risk factors:
Factors that put you at risk of developing trigger finger include:
- Repeated gripping. Occupations and hobbies that involve repetitive hand use and prolonged gripping may increase your risk of trigger finger.
- Certain health problems. People who have diabetes or rheumatoid arthritis are at higher risk of developing trigger finger.
- Your sex. Trigger finger is more common in women.
- Carpal tunnel syndrome surgery. Trigger finger may be a complication associated with surgery for carpal tunnel syndrome surgery, especially during the first six months after surgery.

My Examination
I will be able to diagnose a trigger finger by talking with you about your symptoms and examining your hand. I may order X-rays to look for any underlying issues such as arthritis.
During the exam, I will look for:
- Tenderness over the flexor tendon sheath in the palm of your hand
- Thickening or swelling of the tendon sheath
- Triggering when you bend and straighten your finger
- Difficulty bending your finger
Treatment:
Nonsurgical Treatment
Initial treatment for a trigger finger is usually nonsurgical.
Rest. Resting your hand and avoiding activities that make it worse may be enough to resolve the problem.
Splinting. Wearing a splint at night to keep the affected finger or thumb in a straight position while you sleep may be helpful.
Exercises. Gentle stretching exercises can help decrease stiffness and improve range of motion in the involved digit.
Medications. Over-the-counter medications, such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), can help relieve pain and inflammation.
Steroid injections. Corticosteroid, or cortisone, is an anti-inflammatory agent that can be injected into the tendon sheath at the base of the trigger finger. A steroid injection may resolve the triggering over a period of one day to several weeks. If the symptoms resolve there is the potential for a recurrence, typically months later. If symptoms do not improve with time or return, a second injection may be given. If two injections do not help the problem permanently, surgery may be considered.
Steroid injections are less likely to be effective in patients with diabetes but may still help avoid surgery. They can cause a short-term rise in blood sugar, so glucose levels in diabetic patients should be monitored after injection.

Surgical Treatment:
If your finger does not get better with nonsurgical treatment, you may wish to consider surgery. Surgery is elective. The decision for surgery is based on how much pain or loss of function you have in your finger. If, however, your finger or thumb is stuck in a flexed or bent position, I may recommend surgery to prevent permanent stiffness.
Surgical procedure. The surgical procedure for trigger finger is called “tenolysis” or “trigger finger release.”
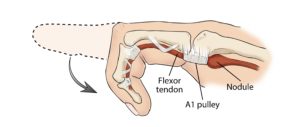
The goal of the procedure is to release the A1 pulley that is blocking tendon movement so the flexor tendon can glide more easily through the tendon sheath. Typically, the procedure is done in an outpatient setting with an injection of local anesthesia to numb the area for surgery.
Surgery is performed through either a small open incision in the palm (my technique) or with the tip of a needle. The A1 pulley is divided (released) so that the flexor tendon can glide freely. Although pulleys have an important function in the hand, releasing the A1 pulley should not cause problems in the future.
Complications:
Complications can occur with any type of surgery. I will discuss the risks with you before surgery and will take specific measures to help prevent complications.
The most common complications following surgery for trigger finger or trigger thumb include:
- Stiffness in the involved finger.
- Inability to straighten the involved finger. If you were not able to straighten your finger completely before surgery, you might not be able to do so afterward.
- Temporary soreness or swelling at the site of surgery
Less common complications include:
- Persistent locking or clicking. This may indicate that more of the pulley needs to be released or may be caused by another problem in your finger.
- “Bowstringing.” In a small number of cases, the tendon may “bow” away from the bone, resulting in reduced range of motion. Bowstringing occurs when one of the more important pulleys is released.
- Infection (rare)
- Digital nerve injury. This may cause numbness or tingling along part of the finger.
Recovery:
I encourage most of my patients to move their finger immediately after surgery.
It is common to have some soreness in your palm. Elevating your hand above your heart can help reduce pain and swelling.
Although your incision will heal within a few weeks (sutures out in 7-10 days), it may take from 4 to 6 months for swelling and stiffness in your hand and fingers or thumb to go away completely.
If stiffness, swelling, or pain persist after surgery, I typically recommend seeing a hand therapist.
Outcome:
Patients who have surgery experience significant improvement in function as well as relief from the pain of a trigger finger. Still, if a contracture or loss of motion was present before surgery, complete range of motion may not be restored.
If you feel as if you or any of your family and friends could have any of the symptoms provided here, medical care is available. I am ready and happy to help you keep your hands healthy and functional.
Thank you,
Ayisha Livingstone, MD
Fellowship Trained and Board-Certified Orthopedic Hand Surgeon
South Florida Orthopedic Group
(954) 771-8177
Learn more about Dr Ayisha E. Livingstone
